Digital Twins in Medicine: How AI is Creating Virtual Patients for Personalized Treatment
When Dr. Elena Rodriguez needed to decide which chemotherapy cocktail to prescribe for her patient with stage 3 lung cancer, she did something that would have been impossible five years ago.
She tested it on a virtual clone first.
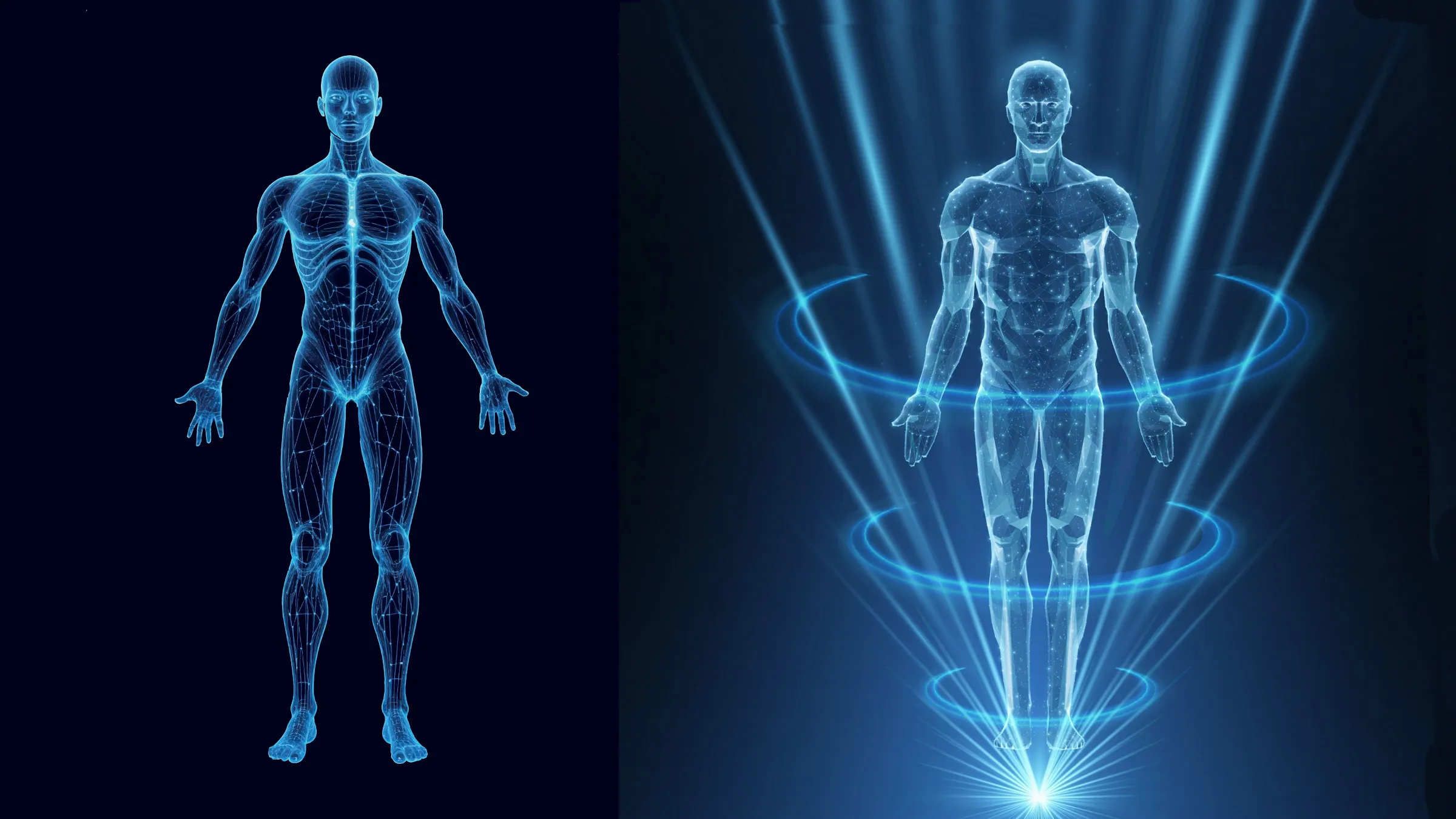
Not a statistical model. Not a population average. A digital replica of her actual patient—complete with his genetic markers, metabolic rates, tumor characteristics, and even his cardiovascular quirks. She ran simulations. Watched how the virtual patient responded. Adjusted dosages. Tried different drug combinations. All before the real patient received a single infusion.
Welcome to the era of digital twins in medicine.
What Is a Medical Digital Twin?
Imagine a video game character that mimics you perfectly. Not just how you look, but how your heart pumps, how your liver metabolizes medications, how your immune system responds to threats. That’s essentially a medical digital twin—a dynamic, computational model that replicates an individual patient’s physiology.
These aren’t static snapshots. They evolve continuously, fed by streams of real-world data from wearables, lab tests, medical imaging, and electronic health records. When your blood pressure changes, your digital twin’s blood pressure changes. When you start a new medication, the twin takes it too—virtually.
The concept borrows from aerospace and manufacturing, where engineers have used digital twins for decades to test aircraft designs and optimize factory production. But applying it to the chaotic, infinitely complex human body? That’s exponentially harder.
And yet, it’s happening.
Testing Treatments Before They Touch You
Robert Martinez, 58, was facing a difficult decision. He’d been diagnosed with atrial fibrillation, an irregular heartbeat that increases stroke risk. His cardiologist recommended a catheter ablation—a procedure that burns away misfiring heart tissue.
But Robert had unusual anatomy. His heart chambers were slightly enlarged. He’d had previous cardiac surgery. Standard protocols might not work, and complications could be serious.
So his medical team at Massachusetts General Hospital created a digital twin of Robert’s heart using MRI scans, electrical mapping data, and AI modeling. They ran the ablation procedure virtually. Multiple times. Testing different ablation points. Predicting which approach would maximize success while minimizing damage to healthy tissue.
When Robert underwent the real procedure, his surgeon followed the route mapped out by his digital twin. The operation succeeded. Recovery was faster than expected. And Robert avoided a potentially dangerous complication the simulations had flagged.
“They practiced on fake-me first,” Robert jokes. “Fake-me did great, so real-me had a chance.”
The Promise: Truly Personalized Medicine
Here’s why doctors are excited about this technology. For decades, medicine has relied on population averages. Clinical trials test drugs on thousands of people, establish that a treatment works for most patients, and then doctors prescribe it hoping you’re in the “most” category.
But you’re not average. Your metabolism might process drugs twice as fast as typical. Your genetic variants might make a standard medication ineffective—or toxic. Your specific tumor might have mutations that make it resistant to first-line chemotherapy.
Digital twins promise to make medicine truly personal. Instead of “this drug works for 70% of patients with your condition,” doctors could say “according to your digital twin, this drug will reduce your tumor by 40% with minimal side effects, but this alternative would work better for you specifically.”
Dr. Jennifer Wong, who leads a digital twin research program at Stanford, describes a recent case. “We had a diabetic patient whose blood sugar was dangerously unstable despite standard insulin protocols. We built her digital twin, incorporated her activity patterns, stress levels, sleep data—everything. The twin revealed she was ultra-sensitive to insulin at certain times of day. We adjusted her dosing schedule based on the simulation. Her glucose control improved dramatically.”
Could they have figured this out through trial-and-error? Maybe. Eventually. But the digital twin compressed months of dangerous experimentation into days of safe simulation.
The Pilots Are Producing Results
This isn’t science fiction. Multiple hospitals are running digital twin pilot programs right now.
The Visible Heart Lab at the University of Minnesota has created cardiac twins for dozens of patients, helping surgeons plan complex procedures. Researchers at Johns Hopkins are using digital twins to optimize radiation therapy for cancer patients—simulating different beam angles and dosages to maximize tumor destruction while sparing healthy tissue.
In Europe, the INSILICO project is building digital twins for drug discovery, simulating how new compounds interact with virtual patients before human trials begin. Early results suggest they can identify promising candidates faster and eliminate dangerous drugs earlier.
The outcomes are encouraging. One study found that using cardiac digital twins for ablation planning improved success rates by 15% and reduced complications by 22%. Another showed that digital twin-guided chemotherapy reduced severe side effects by 30% while maintaining efficacy.
The Challenges Are Enormous
But let’s be honest about the obstacles. Building an accurate digital twin of a human body is absurdly complicated.
Your body contains roughly 37 trillion cells. Multiple organ systems interact in ways we still don’t fully understand. Genetic expression changes based on environment, stress, diet, sleep, and factors we can’t even measure. Creating a model that captures this complexity requires massive computational power and data we often don’t have. That’s why we need AI development.
Current digital twins focus on specific organs or systems—a heart twin, a lung twin, a tumor twin. Creating a whole-body twin that accurately simulates multi-system interactions? We’re years away from that.
There’s also the data problem. Building an accurate twin requires enormous amounts of patient data—genomic sequencing, continuous monitoring, detailed imaging, metabolic testing. Collecting this data is expensive, invasive, and time-consuming. Most patients don’t have comprehensive enough records to build truly accurate twins.
And then there’s validation. How do you prove a digital twin is accurate? You can’t easily compare its predictions against real outcomes without actually trying different treatments on the real patient—which defeats the purpose.
The Ethics Get Complicated Fast
Dr. Michael Osei, a medical ethicist at Yale, raises uncomfortable questions. “Who owns your digital twin? Can your insurance company create one and use it to predict future health problems—then raise your rates? Can pharmaceutical companies access twins for drug testing without patient consent? What if your twin reveals genetic risks you didn’t want to know about?”
There’s also the question of access. Building digital twins is expensive and technologically sophisticated. Will this become another medical advance available only to wealthy patients at elite hospitals? Or can it scale to serve everyone?
And perhaps most troubling—what happens when doctors trust the model more than their clinical judgment? Digital twins are tools, not oracles. They’re only as good as their data and algorithms. A twin might miss rare complications, unusual patient responses, or factors it wasn’t designed to consider.
“We need doctors who can interpret and question these models,” Dr. Osei says. “Not just follow them blindly.”
What Comes Next
Despite the challenges, momentum is building. The FDA is developing regulatory frameworks for digital twin applications. Tech giants and startups are investing billions. More hospitals are launching pilot programs.
Within five years, Dr. Wong predicts digital twins will be routine for complex surgeries and cancer treatment planning. Within ten, they might guide chronic disease management for millions of patients.
Robert Martinez, the heart patient, has stayed in touch with his medical team. His digital twin still exists, continuously updated with data from his smartwatch and regular checkups. If his atrial fibrillation returns, his doctors won’t start from scratch—they’ll consult his twin, which now has years of post-procedure data.
“It’s weird knowing fake-me exists somewhere,” Robert says. “But fake-me might save real-me’s life someday. So I’m okay with it.”
In medicine’s future, we might all have a digital doppelganger. A virtual twin that gets sick first, tests treatments first, takes risks first.
So we don’t have to.
Keep an eye for more latest news & updates on NY Heading!